Accidents happen. We’re here to help you.
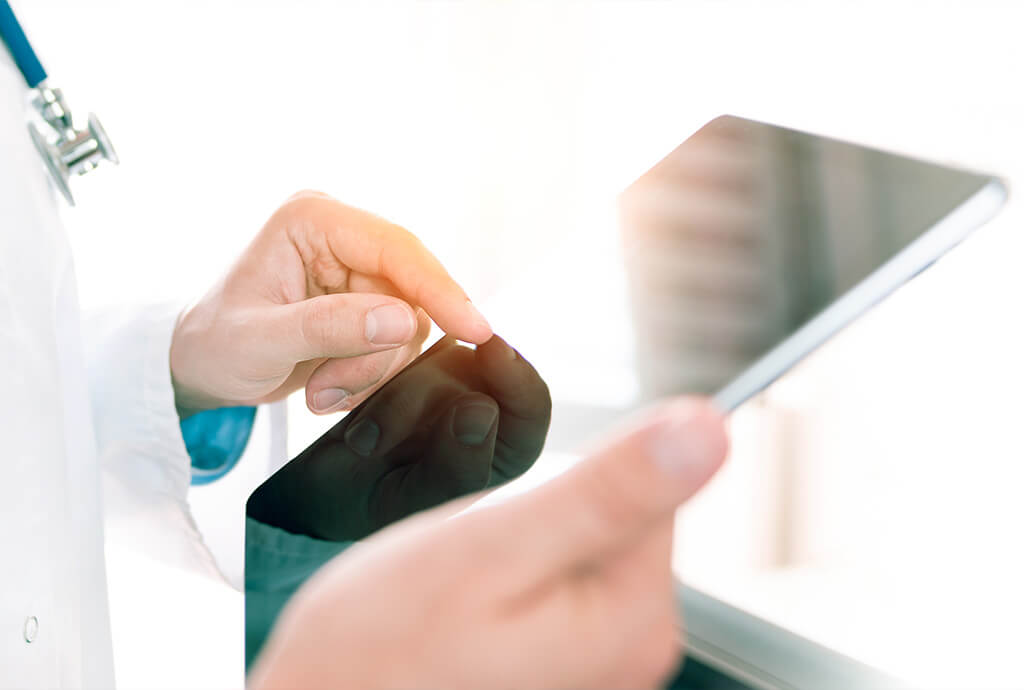
When an employee is injured on the job, KEMI is ready to help you navigate the claim process and provide the highest standard of care available to the claimant throughout the claim. Learn how KEMI helps you manage claims, check out our frequently asked questions below, or contact us if you have specific claims questions.
Report an incident or illness immediately.
Guide the claimant on seeking initial medical treatment.
Provide KEMI with requested wage information.
Take corrective action if possible to prevent future incidents.
Submitting a First Report of Incident
Submit the First Report of Incident or Illness online for the quickest and easiest way to report a claim.
A claim may also be reported by:
- Email – complete First Report of Incident or Illness (IA-1 form) and email to claim@kemi.com.
- Fax – complete the First Report of Incident or Illness and fax to 859-425-7822.
- Phone – call 800-640-KEMI (5364) during business hours Monday – Friday from 8 a.m.-5 p.m. Eastern time.
- Mail – print and complete the First Report of Incident or Illness and mail to:
KEMI
ATTN: Claims Unit
P.O. Box 12500
Lexington, KY 40583-2500
The Claims Process
Once an incident is reported to KEMI, our Claims Team will move into action by reviewing the information and ensuring the claimant receives the care they deserve. Reporting the claim isn’t just good practice; it’s the law. KRS 342.038 requires policyholders to report injuries or illnesses to us within three (3) working days of receiving notification of the incident or alleged incident.
Once we’ve reviewed the First Report of Incident, we will request additional information from you as we determine appropriate benefits for the claimant. If the claimant needs ongoing treatment, please refer them to our Managed Care Network. If the claimant is able to return to work with restrictions, we will work with the you to make those accommodations if possible.
As part of our commitment to you, we want to help your employee return to work as quickly and safely as possible.
Resources for Employers
KEMI works closely with the Occupational Managed Care Network (OMCA) to provide quality care for work-related injuries.
Both policyholders and claimants benefit from KEMI’s extensive claims management tools and resources. These resources include a Pharmacy Benefit Management (PBM) Program to monitor prescription drug trends, and a medical bill review program to identify duplicate billing and coding errors.
Additional Resources
The following resources highlight several of the benefits policyholders receive when choosing KEMI for their workers’ compensation coverage.
Claims Detail Dashboard
Policyholders may login to access important claims details using our interactive Claims Detail Dashboard.
login or registerManaged Care Network
KEMI’s Managed Care Network through OMCA provides claimants with quality care.
Learn about Managed CarePharmacy Benefits Manager
Our PBM program by Mitchell helps control prescription costs which helps lower the overall premium of the policy.
How We control Rx CostsMedical Bill Auditing
Our Medical Bill Team makes sure provider services are adjusted to the fee schedule and paid appropriately.
Learn about our processLoss Control & Safety
Our Claims Team works closely with our Loss Control & Safety Team to investigate and prevent injuries.
ACCESS FREE SAFETY RESOURCESMedcor
KEMI has partnered with Medcor to provide you with an extra level of service when claims arise.
Register for medcorKEMI has a zero-tolerance policy on workers’ compensation fraud to protect our policyholders and their employees. Report fraud.
Frequently Asked Questions
Work-related injuries and illnesses should be reported to KEMI immediately. Kentucky law states that policyholders must report injuries or illnesses to us within three (3) working days of receiving notification of the incident or alleged incident.
The fastest and easiest way to report an injury or illness is through submitting the First Report of Injury online. A claim may also be reported by printing the First Report of Injury or Illness, or IA-1 form, and faxing it to 859-425-7822 or mailing to the address below:
KEMI
ATTN: Claims Unit
P.O. Box 12500
Lexington, KY 40583-2500
To report a claim by phone, call 1-800-640-KEMI (5364) or 859-425-7800 during business hours (Monday – Friday from 8 a.m.-5 p.m.).
KEMI has partnered with OMCA, a managed care network, which has medical providers throughout Kentucky.
ACCESS THE OMCA PROVIDER LISTIf you have questions or wish to recommend a new provider to the list, contact us.
The claim process for an employer is as follows:
- Report the injury to KEMI immediately.
- Guide the injured worker to seek initial treatment. For emergencies where loss of life or limb is a concern, call 9-1-1 or go to the nearest hospital. For non-life threatening injuries or illnesses, find a list of providers here.
- KEMI will assign the claim to an examiner, who will then review the claim and determine if it is approved or denied in accordance with state law.
- If the claim is approved, we will provide you with a claim number for future reference.
- A claims examiner will request information from the policyholder regarding wages, employment, details about the incident, etc.
- We will work with the injured worker and medical providers to ensure appropriate care and benefits are provided.
- We may also communicate with the policyholder regarding the status of open claims.
- If you receive any work or medical notes related to the claim, please provide a copy of them to the claims examiner.
- Accommodate restrictions for the injured worker if possible to allow them to return to work.
- Once the injured worker returns to work and has been released from medical treatment at maximum medical improvement, the claim may be administratively closed.
Policyholders can view claim status and policy details on KEMI.com if they are registered and signed in to our secure portal. Sign in now or learn more about becoming a registered user.
Additionally, if you have questions about a claim you may contact the KEMI claims examiner at 1-800-640-KEMI (5364) or 859-425-7800. You may also use the contact form here.
Claims Forms
- IA-1 First Report of Incident
- Direct Deposit
- Direct Deposit (Spanish)
- Average Weekly Wage Certification (AWW)
- Medical Waiver & Consent Form (Form 106)
- Notice of Designated Physician (Form 113)
- Claimant Reimbursement Form (Form 114)
- Job Analysis Form
- W-9 Taxpayer Identification Number Request Form (IRS Website)
Still have questions?
If you have a claims question, give us a call at 1-800-640-KEMI (5364) or 859-425-7800. You may also use the contact form here.